
Our revolutionary DigiLum™ solution closes the loop on PDT light activation, enabling a new paradigm in precision PDT administration and effectiveness.
Combining advanced AI-driven photonics instrumentation with a next-generation photosensitizer agent, the DigiLum system is a powerful platform is readily adoptable to unlock the potential of PDT to treat a broader
range of cancer sites and extend the benefits of this more tolerable therapy to a greater number of patients.
Our photonics system is based on innovative optical surface applicator device technology demonstrated by Roswell Park Cancer Center that allows direct measurement of light interaction with target tissue. This enables automated, real-time light monitoring and
closed loop control of PDT light delivery.
Furthermore, this technology allows integration of multiple light emitter/detector fiber optics over a broad area to greatly reduce intraoperative PDT procedure time- from hours to minutes.
Our system sets a new benchmark of sophistication in PDT light administration through proprietary machine learning algorithms that factor target tissue optical properties and light propagation effects of different media in the procedure setting to deliver an unprecedented level of precision in PDT light dosimetry. Our DigiLum™ system represents the first true PDT light dosimetry
system based on real-time data that is fully automated for ease of use, eliminating operator dependencies for repeatable, reliable clinical results.
Our revolutionary DigiLum™ solution presents a new paradigm in PDT administration and effectiveness, combining advanced AI-driven photonics instrumentation with a next-generation photosensitizer agent. This powerful platform is readily adoptable to unlock the potential of PDT to treat a broader range of cancer sites and extend the benefits of this more tolerable therapy to a greater number of patients.
Closing The Loop on PDT Light Activation
Our photonics system is based on innovative optical surface applicator device technology demonstrated by Roswell Park Cancer Center that allows direct measurement of light interaction with target tissue. This enables automated, real-time light monitoring and closed loop control of PDT light delivery. Furthermore, this technology allows integration of multiple light emitter/detector fiber optics over a broad area to greatly reduce intraoperative PDT procedure time- from hours to minutes.
Our system sets a new benchmark of sophistication in PDT light administration through proprietary machine learning algorithms that factor target tissue optical properties and light propagation effects of different media in the procedure setting to deliver an unprecedented level of precision in PDT light dosimetry. Our DigiLum™ system represents the first true PDT light dosimetry system based on real-time data that is fully automated for ease of use, eliminating operator dependencies for repeatable, reliable clinical results.
5-Aminolevulinic Acid (5-ALA)- The Ideal Photosensitizer
While our DigiLum™ system can be designed to activate any photosensitizer, our focus is on use of 5-aminolevulinic acid (5-ALA), a next generation photosensitizer with a known safety profile that is highly selective to tumor tissue for minimum off-target effects with negligible post-procedure phototoxicity- 24 hours compared to 30+ day of the current approved agent used in lung cancer. It offers a short time between drug administration and light activation that is more amenable to surgical procedure workflows.
Marketed in the US as Gleolan™, it is currently approved in 42 countries as an imaging agent for fluorescence-guided glioma surgery. Gleolan™ presents the unique potential beyond imaging to also be used as a therapeutic agent, enabling intraoperative “see and treat” applications during surgical procedures.
Endogenous PplX
Cancer cells that have absorbed excess amounts of 5-ALA are unable to produce herme properly and accumulate PplX in cell mitochondrion, where it can be exploited by illumination for diagnostic PPD (blue light-fluorescence) or therapeutic PDT (red light-reactive oxygen species (ROS) generation.
5-ALA is produced naturally in the body and processed into protoporphyrin IX (PplX), a powerful photosensitizer used in heme synthesis.
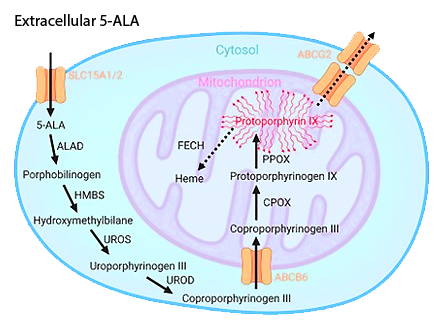
Sourch: Mischkulnig et al.2022 Dol 10.3389/med2022.907442
Mitochondria-targeted PDT is considered highly efficient in cell killing and can induce multiple signal transduction passways and effector responses, making it ideal for immunogenic PDT.
5-ALA/Endogenous PplX offers higher selectivity to disease tissue and minimum phototoxicity (<24hr) compared to other photosensitizers.
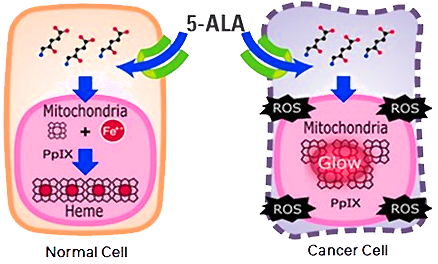
Sourch: SBI Pharmaceuticals Co., Ltd.
5-Aminolevulinic Acid (5-ALA) – The Ideal Photosensitizer
While our DigiLum™ system can be designed to activate any photosensitizer, our focus is on use of 5-aminolevulinic acid (5-ALA), a next generation photosensitizer with a known safety profile that is highly selective to tumor tissue for minimum off-target effects with negligible post-procedure phototoxicity- 24 hours compared to 30+ day of the current approved agent used in lung cancer. It offers a short time between drug administration and light activation that is more amenable to surgical procedure workflows.
Marketed in the US as Gleolan™, it is currently approved in 42 countries as an imaging agent for fluorescence-guided glioma surgery. Gleolan™ presents the unique potential beyond imaging to also be used as a therapeutic agent, enabling intraoperative “see and treat” applications during surgical procedures.

A light applicator inserted in patient

Applicator positioned, secured
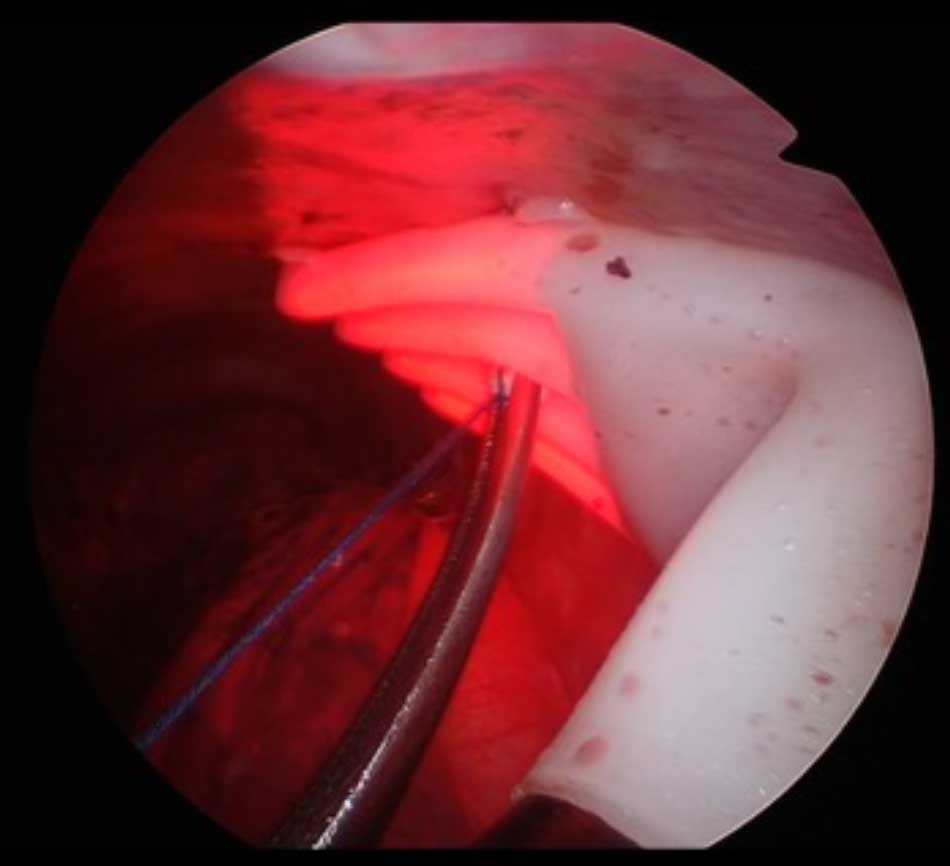
Touchscreen start, automated light delivery
Unlocking the Power of PDT with the Revolutionary DigiLum™ System for Enhanced Cancer Treatment
Discover how our innovative DigiLum™ system is transforming the landscape of Photodynamic Therapy (PDT) by expanding its application to various cancer sites and intraoperative surgical settings. This groundbreaking system allows us to deliver a proven therapy to a larger patient population, ensuring comprehensive treatment options.
The Benefits of PDT: Mechanism of Action and Clinical Outcomes
PDT operates through a unique mechanism of action that induces oxidative stress without toxic side effects. This advanced approach enables a range of clinical outcomes, including effective tumor ablation, immunogenic cell death, and local tumor control for patients undergoing surgical resection. Unlike traditional therapies, PDT is tumor-agnostic, showing no signs of acquired resistance. It works seamlessly with other treatments, ensuring minimal damage to healthy tissue for optimal cosmetic and organ function preservation.
At OncoLux, we are at the forefront of pioneering new indications for PDT as a more tolerable, effective, and toxicity-free alternative to chemotherapy and radiotherapy.
Local Treatment with a Systemic Response: Enhancing Immunotherapy Efficacy
Our initial focus for the DigiLum™ system highlights the application of PDT as an immune adjuvant therapy, specifically designed to enhance the response rates of patients suffering from advanced lung cancer who are receiving standard immune checkpoint blockade therapies. Our targeted approach selectively destroys local tumor cells while simultaneously empowering the immune system to identify and eradicate both residual and distant cancerous cells.
In contrast to other immunogenic cell death methods, such as chemotherapy and radiotherapy, which can be indiscriminate and immunosuppressive, our PDT strategy preserves essential immune components, eliminating toxic side effects and severe reactions.
Advancing PDT for Lung Cancer and Pleural Disease
Our mission at OncoLux is clear: to refine and promote PDT as a more effective and tolerable treatment option, particularly when combined with immunotherapy for patients battling lung cancer and pleural disease. Join us in revolutionizing cancer treatment through the power of innovative PDT strategies with the DigiLum™ system.
